http://www.thorne.com/altmedrev/.fulltext/4/4/272.pdf
Am J Gastroenterol. 1998 Feb;93(2):139-43. Related Articles, Links
Comment in:
[SIZE=+1]Milk thistle (Silybum marianum) for the therapy of liver disease.[/SIZE]
Flora K, Hahn M, Rosen H, Benner K.
Division of Gastroenterology, Oregon Health Sciences University, Portland 97201-3098, USA.
Silymarin, derived from the milk thistle plant, Silybum marianum, has been used for centuries as a natural remedy for diseases of the liver and biliary tract. As interest in alternative therapy has emerged in the United States, gastroenterologists have encountered increasing numbers of patients taking silymarin with little understanding of its purported properties. Silymarin and its active constituent, silybin, have been reported to work as antioxidants scavenging free radicals and inhibiting lipid peroxidation. Studies also suggest that they protect against genomic injury, increase hepatocyte protein synthesis, decrease the activity of tumor promoters, stabilize mast cells, chelate iron, and slow calcium metabolism. In this article we review silymarin's history, pharmacology, and properties, and the clinical trials pertaining to patients with acute and chronic liver disease.
Publication Types:PMID: 9468229 [PubMed - indexed for MEDLINE]
[SIZE=+1]Silymarin retards the progression of alcohol-induced hepatic fibrosis in baboons.[/SIZE]
Lieber CS, Leo MA, Cao Q, Ren C, DeCarli LM.
Section of Liver Disease & Nutrition, Bronx VA Medical Center & Mount Sinai School of Medicine, Bronx, New York 10468, USA. [email protected]
GOAL/BACKGROUND: Hepatoprotective effects of silymarin in patients with alcoholic liver disease are controversial. For strict control, this was assessed in non-human primates.STUDY Twelve baboons were fed alcohol with or without silymarin for 3 years with a nutritionally adequate diet. RESULTS: Silymarin opposed the alcohol-induced oxidative stress (assessed by plasma 4-hydroxynonenal) and the rise in liver lipids and circulating ALT. Alcohol also increased hepatic collagen type I by 50% over the 3 years with a significant rise in mRNA for alpha1 (I) procollagen, both prevented by silymarin. There were corresponding morphologic changes: at 36 months, 2 of 6 animals fed alcohol had cirrhosis and 2 septal fibrosis, with perivenular fibrosis in 2, whereas with alcohol + silymarin, there was only 1 cirrhosis and 1 septal fibrosis, with perivenular fibrosis in 2, and virtually no lesions in the remaining 2. CONCLUSIONS: Silymarin retards the development of alcohol-induced hepatic fibrosis in baboons, consistent with several positive clinical trials. The negative outcome observed in other trials possibly reflects poor compliance resulting in irregular or low silymarin intake. Thus, in view of the innocuity of silymarin, it might be advisable in future clinical studies to insure the controlled administration of sufficient amounts of silymarin.
[SIZE=+1]Effect of silybin and its congeners on human liver microsomal cytochrome P450 activities.[/SIZE]
Zuber R, Modriansky M, Dvorak Z, Rohovsky P, Ulrichova J, Simanek V, Anzenbacher P.
Faculty of Chemical Technology, University of Pardubice, Nam. Cs. Legii 565, 532 10 Pardubice, Czech Republic.
Silybin and related flavonolignans form a major part of the Silybum marianum extract, silymarin, which has been used to treat liver diseases for hundreds of years. Although regarded as safe, many of the extract constituents remain thus far untested for their possible effects on liver biotransformation enzymes. Cytochromes P450 (CYP) are very important in this regard. We tested the effect of four flavonolignans: silybin, its hemisynthetic derivative dehydrosilybin, silydianin, and silycristin on three specific CYP activities: bufuralol 1'-hydroxylation (CYP2D6), p-nitrophenol hydroxylation (CYP2E1), and nifedipine oxidation (CYP3A4). All flavonolignans displayed dose-dependent inhibition of these activities with IC(50) values in the micromolar range. The inhibition was competitive or mixed as revealed by double reciprocal plots of kinetic experiments. However, the inhibition is not considered to be relevant for therapy because physiological concentrations of the individual flavonolignans do not exceed 0.5 microM. The data support the use of the extract as a dietary supplement. Copyright 2002 John Wiley & Sons, Ltd.
PMID: 12410543 [PubMed - indexed for MEDLINE]
[SIZE=+1]The use of silymarin in the treatment of liver diseases.[/SIZE]
Saller R, Meier R, Brignoli R.
Abteilung Naturheilkunde, University Hospital Zurich, Switzerland.
The high prevalence of liver diseases such as chronic hepatitis and cirrhosis underscores the need for efficient and cost-effective treatments. The potential benefit of silymarin (extracted from the seeds of Silybum marianum or milk thistle) in the treatment of liver diseases remains a controversial issue. Therefore, the objective of this review is to assess the clinical efficacy and safety of silymarin by application of systematic approach. 525 references were found in the databases, of which 84 papers were retained for closer examination and 36 were deemed suitable for detailed analysis. Silymarin has metabolic and cell-regulating effects at concentrations found in clinical conditions, namely carrier-mediated regulation of cell membrane permeability, inhibition of the 5-lipoxygenase pathway, scavenging of reactive oxygen species (ROS) of the R-OH type and action on DNA-expression, for example, via suppression of nuclear factor (NF)-kappaB. Pooled data from case record studies involving 452 patients with Amanita phalloides poisoning show a highly significant difference in mortality in favour of silibinin [the main isomer contained in silymarin] (mortality 9.8% vs 18.3% with standard treatment; p < 0.01). The available trials in patients with toxic (e.g. solvents) or iatrogenic (e.g. antispychotic or tacrine) liver diseases, which are mostly outdated and underpowered, do not enable any valid conclusions to be drawn on the value of silymarin. The exception is an improved clinical tolerance of tacrine. In spite of some positive results in patients with acute viral hepatitis, no formally valid conclusion can be drawn regarding the value of silymarin in the treatment of these infections. Although there were no clinical end-points in the four trials considered in patients with alcoholic liver disease, histological findings were reported as improved in two out of two trials, improvement of prothrombin time was significant (two trials pooled) and liver transaminase levels were consistently lower in the silymarin-treated groups. Therefore, silymarin may be of use as an adjuvant in the therapy of alcoholic liver disease. Analysis was performed on five trials with a total of 602 patients with liver cirrhosis. The evidence shows that, compared with placebo, silymarin produces a nonsignificant reduction of total mortality by -4.2% [odds ratio (OR) 0.75 (0.5 - 1.1)]; but that, on the other hand, the use of silymarin leads to a significant reduction in liver-related mortality of-7% [OR: 0.54 (0.3 - 0.9); p < 0.01]. An individual trial reported a reduction in the number of patients with encephalopathy of -8.7% (p = 0.06). In one study of patients with cirrhosis-related diabetes mellitus, the insulin requirement was reduced by -25% (p < 0.01). We conclude that available evidence suggests that silymarin may play a role in the therapy of (alcoholic) liver cirrhosis. Silymarin is has a good safety record and only rare case reports of gastrointestinal disturbances and allergic skin rashes have been published. This review does not aim to replace future prospective trials aiming to provide the 'final' evidence of the efficacy of silymarin.
Publication Types:PMID: 11735632 [PubMed - indexed for MEDLINE]
[SIZE=+1]New treatments for hepatitis B and C [antigen-specific transfer for A, B & C (chisolm biologicals) and thymate].[/SIZE]
Konlee M.
AIDS: Millions of people in this country are infected with Hepatitis C; however, long-term treatment for this disease is not always successful. Chisolm Biologicals produces a transfer factor panel for hepatitis A, B, and C that appears to be effective in treating hepatitis. Other products, including Thy-Mate and Liver Support, may also help treat hepatitis. Patients with hepatitis should tell their doctor what products they are using and have their physicians monitor liver enzyme levels and viral loads. One study of 24 patients showed success in using Naltrexone, Alpha Lipoic acid, milk thistle, and Hypercurium in treating hepatitis B and C. Contact information is included.
Publication Types:PMID: 11366548 [PubMed - indexed for MEDLINE]
Altern Med Rev. 1998 Dec;3(6):410-21. Related Articles, Links
[SIZE=+1]A review of plants used in the treatment of liver disease: part 1.[/SIZE]
Luper S.
Southwest College of Naturopathic Medicine: 2140 East Broadway Rd. Tempe, AZ 85282, USA. [email protected]
Botanicals have been used traditionally by herbalists and indigenous healers worldwide for the prevention and treatment of liver disease. Clinical research in this century has confirmed the efficacy of several plants in the treatment of liver disease. Basic scientific research has uncovered the mechanisms by which some plants afford their therapeutic effects. Silybum marianum (milk thistle) has been shown to have clinical applications in the treatment of toxic hepatitis, fatty liver, cirrhosis, ischemic injury, radiation toxicity, and viral hepatitis via its antioxidative, anti-lipid peroxidative, antifibrotic, anti-inflammatory, immunomodulating, and liver regenerating effects. Picrorhiza kurroa, though less well researched than Silybum, appears to have similar applications and mechanisms of action. When compared with Silybum, the hepatoprotective effect of Picrorhiza was found to be similar, or in many cases, superior to the effect of Silybum.
Publication Types:
PMID: 9855566 [PubMed - indexed for MEDLINE] Altern Med Rev. 1999 Jun;4(3):178-88. Related Articles, Links
[SIZE=+1]A review of plants used in the treatment of liver disease: part two.[/SIZE]
Luper S.
Southwest College of Naturopathic Medicine: 2140 East Broadway Rd. Tempe, AZ 85282, USA. [email protected]
Botanical medicines have been used traditionally by herbalists and indigenous healers worldwide for the prevention and treatment of liver disease. Clinical research in this century has confirmed the efficacy of several plants in the treatment of liver disease, while basic scientific research has uncovered the mechanisms by which some plants provide their therapeutic effects. This article is Part Two in a review of botanicals used in the treatment of liver disease. Curcuma longa (turmeric), Camellia sinensis (green tea), and Glycyrrhiza glabra (licorice) are reviewed in this installment. Silybum marianum (milk thistle) and Picrorhiza kurroa (kutkin) were reviewed in Part One.
Publication Types:
PMID: 10383482 [PubMed - indexed for MEDLINE]
The 2 last ones (in italics) would be VERY nice to get a hold of, just to extract the conclusions on Milk Thistle...
Am J Gastroenterol. 1998 Feb;93(2):139-43. Related Articles, Links
Comment in:

[SIZE=+1]Milk thistle (Silybum marianum) for the therapy of liver disease.[/SIZE]
Flora K, Hahn M, Rosen H, Benner K.
Division of Gastroenterology, Oregon Health Sciences University, Portland 97201-3098, USA.
Silymarin, derived from the milk thistle plant, Silybum marianum, has been used for centuries as a natural remedy for diseases of the liver and biliary tract. As interest in alternative therapy has emerged in the United States, gastroenterologists have encountered increasing numbers of patients taking silymarin with little understanding of its purported properties. Silymarin and its active constituent, silybin, have been reported to work as antioxidants scavenging free radicals and inhibiting lipid peroxidation. Studies also suggest that they protect against genomic injury, increase hepatocyte protein synthesis, decrease the activity of tumor promoters, stabilize mast cells, chelate iron, and slow calcium metabolism. In this article we review silymarin's history, pharmacology, and properties, and the clinical trials pertaining to patients with acute and chronic liver disease.
Publication Types:PMID: 9468229 [PubMed - indexed for MEDLINE]
[SIZE=+1]Silymarin retards the progression of alcohol-induced hepatic fibrosis in baboons.[/SIZE]
Lieber CS, Leo MA, Cao Q, Ren C, DeCarli LM.
Section of Liver Disease & Nutrition, Bronx VA Medical Center & Mount Sinai School of Medicine, Bronx, New York 10468, USA. [email protected]
GOAL/BACKGROUND: Hepatoprotective effects of silymarin in patients with alcoholic liver disease are controversial. For strict control, this was assessed in non-human primates.STUDY Twelve baboons were fed alcohol with or without silymarin for 3 years with a nutritionally adequate diet. RESULTS: Silymarin opposed the alcohol-induced oxidative stress (assessed by plasma 4-hydroxynonenal) and the rise in liver lipids and circulating ALT. Alcohol also increased hepatic collagen type I by 50% over the 3 years with a significant rise in mRNA for alpha1 (I) procollagen, both prevented by silymarin. There were corresponding morphologic changes: at 36 months, 2 of 6 animals fed alcohol had cirrhosis and 2 septal fibrosis, with perivenular fibrosis in 2, whereas with alcohol + silymarin, there was only 1 cirrhosis and 1 septal fibrosis, with perivenular fibrosis in 2, and virtually no lesions in the remaining 2. CONCLUSIONS: Silymarin retards the development of alcohol-induced hepatic fibrosis in baboons, consistent with several positive clinical trials. The negative outcome observed in other trials possibly reflects poor compliance resulting in irregular or low silymarin intake. Thus, in view of the innocuity of silymarin, it might be advisable in future clinical studies to insure the controlled administration of sufficient amounts of silymarin.
[SIZE=+1]Effect of silybin and its congeners on human liver microsomal cytochrome P450 activities.[/SIZE]
Zuber R, Modriansky M, Dvorak Z, Rohovsky P, Ulrichova J, Simanek V, Anzenbacher P.
Faculty of Chemical Technology, University of Pardubice, Nam. Cs. Legii 565, 532 10 Pardubice, Czech Republic.
Silybin and related flavonolignans form a major part of the Silybum marianum extract, silymarin, which has been used to treat liver diseases for hundreds of years. Although regarded as safe, many of the extract constituents remain thus far untested for their possible effects on liver biotransformation enzymes. Cytochromes P450 (CYP) are very important in this regard. We tested the effect of four flavonolignans: silybin, its hemisynthetic derivative dehydrosilybin, silydianin, and silycristin on three specific CYP activities: bufuralol 1'-hydroxylation (CYP2D6), p-nitrophenol hydroxylation (CYP2E1), and nifedipine oxidation (CYP3A4). All flavonolignans displayed dose-dependent inhibition of these activities with IC(50) values in the micromolar range. The inhibition was competitive or mixed as revealed by double reciprocal plots of kinetic experiments. However, the inhibition is not considered to be relevant for therapy because physiological concentrations of the individual flavonolignans do not exceed 0.5 microM. The data support the use of the extract as a dietary supplement. Copyright 2002 John Wiley & Sons, Ltd.
PMID: 12410543 [PubMed - indexed for MEDLINE]
[SIZE=+1]The use of silymarin in the treatment of liver diseases.[/SIZE]
Saller R, Meier R, Brignoli R.
Abteilung Naturheilkunde, University Hospital Zurich, Switzerland.
The high prevalence of liver diseases such as chronic hepatitis and cirrhosis underscores the need for efficient and cost-effective treatments. The potential benefit of silymarin (extracted from the seeds of Silybum marianum or milk thistle) in the treatment of liver diseases remains a controversial issue. Therefore, the objective of this review is to assess the clinical efficacy and safety of silymarin by application of systematic approach. 525 references were found in the databases, of which 84 papers were retained for closer examination and 36 were deemed suitable for detailed analysis. Silymarin has metabolic and cell-regulating effects at concentrations found in clinical conditions, namely carrier-mediated regulation of cell membrane permeability, inhibition of the 5-lipoxygenase pathway, scavenging of reactive oxygen species (ROS) of the R-OH type and action on DNA-expression, for example, via suppression of nuclear factor (NF)-kappaB. Pooled data from case record studies involving 452 patients with Amanita phalloides poisoning show a highly significant difference in mortality in favour of silibinin [the main isomer contained in silymarin] (mortality 9.8% vs 18.3% with standard treatment; p < 0.01). The available trials in patients with toxic (e.g. solvents) or iatrogenic (e.g. antispychotic or tacrine) liver diseases, which are mostly outdated and underpowered, do not enable any valid conclusions to be drawn on the value of silymarin. The exception is an improved clinical tolerance of tacrine. In spite of some positive results in patients with acute viral hepatitis, no formally valid conclusion can be drawn regarding the value of silymarin in the treatment of these infections. Although there were no clinical end-points in the four trials considered in patients with alcoholic liver disease, histological findings were reported as improved in two out of two trials, improvement of prothrombin time was significant (two trials pooled) and liver transaminase levels were consistently lower in the silymarin-treated groups. Therefore, silymarin may be of use as an adjuvant in the therapy of alcoholic liver disease. Analysis was performed on five trials with a total of 602 patients with liver cirrhosis. The evidence shows that, compared with placebo, silymarin produces a nonsignificant reduction of total mortality by -4.2% [odds ratio (OR) 0.75 (0.5 - 1.1)]; but that, on the other hand, the use of silymarin leads to a significant reduction in liver-related mortality of-7% [OR: 0.54 (0.3 - 0.9); p < 0.01]. An individual trial reported a reduction in the number of patients with encephalopathy of -8.7% (p = 0.06). In one study of patients with cirrhosis-related diabetes mellitus, the insulin requirement was reduced by -25% (p < 0.01). We conclude that available evidence suggests that silymarin may play a role in the therapy of (alcoholic) liver cirrhosis. Silymarin is has a good safety record and only rare case reports of gastrointestinal disturbances and allergic skin rashes have been published. This review does not aim to replace future prospective trials aiming to provide the 'final' evidence of the efficacy of silymarin.
Publication Types:PMID: 11735632 [PubMed - indexed for MEDLINE]
[SIZE=+1]New treatments for hepatitis B and C [antigen-specific transfer for A, B & C (chisolm biologicals) and thymate].[/SIZE]
Konlee M.
AIDS: Millions of people in this country are infected with Hepatitis C; however, long-term treatment for this disease is not always successful. Chisolm Biologicals produces a transfer factor panel for hepatitis A, B, and C that appears to be effective in treating hepatitis. Other products, including Thy-Mate and Liver Support, may also help treat hepatitis. Patients with hepatitis should tell their doctor what products they are using and have their physicians monitor liver enzyme levels and viral loads. One study of 24 patients showed success in using Naltrexone, Alpha Lipoic acid, milk thistle, and Hypercurium in treating hepatitis B and C. Contact information is included.
Publication Types:PMID: 11366548 [PubMed - indexed for MEDLINE]
Altern Med Rev. 1998 Dec;3(6):410-21. Related Articles, Links

[SIZE=+1]A review of plants used in the treatment of liver disease: part 1.[/SIZE]
Luper S.
Southwest College of Naturopathic Medicine: 2140 East Broadway Rd. Tempe, AZ 85282, USA. [email protected]
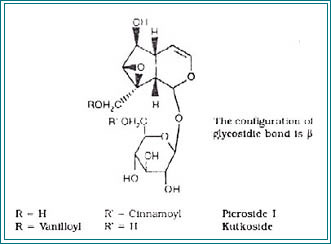
Botanicals have been used traditionally by herbalists and indigenous healers worldwide for the prevention and treatment of liver disease. Clinical research in this century has confirmed the efficacy of several plants in the treatment of liver disease. Basic scientific research has uncovered the mechanisms by which some plants afford their therapeutic effects. Silybum marianum (milk thistle) has been shown to have clinical applications in the treatment of toxic hepatitis, fatty liver, cirrhosis, ischemic injury, radiation toxicity, and viral hepatitis via its antioxidative, anti-lipid peroxidative, antifibrotic, anti-inflammatory, immunomodulating, and liver regenerating effects. Picrorhiza kurroa, though less well researched than Silybum, appears to have similar applications and mechanisms of action. When compared with Silybum, the hepatoprotective effect of Picrorhiza was found to be similar, or in many cases, superior to the effect of Silybum.
Publication Types:
PMID: 9855566 [PubMed - indexed for MEDLINE] Altern Med Rev. 1999 Jun;4(3):178-88. Related Articles, Links

[SIZE=+1]A review of plants used in the treatment of liver disease: part two.[/SIZE]
Luper S.
Southwest College of Naturopathic Medicine: 2140 East Broadway Rd. Tempe, AZ 85282, USA. [email protected]
Botanical medicines have been used traditionally by herbalists and indigenous healers worldwide for the prevention and treatment of liver disease. Clinical research in this century has confirmed the efficacy of several plants in the treatment of liver disease, while basic scientific research has uncovered the mechanisms by which some plants provide their therapeutic effects. This article is Part Two in a review of botanicals used in the treatment of liver disease. Curcuma longa (turmeric), Camellia sinensis (green tea), and Glycyrrhiza glabra (licorice) are reviewed in this installment. Silybum marianum (milk thistle) and Picrorhiza kurroa (kutkin) were reviewed in Part One.
Publication Types:
PMID: 10383482 [PubMed - indexed for MEDLINE]
The 2 last ones (in italics) would be VERY nice to get a hold of, just to extract the conclusions on Milk Thistle...